Congenital Femoral Deficiency (Proximal Femoral Focal Deficiency and Congenital Short Femur)
Elizabeth W. Hubbard, MD
Introduction:
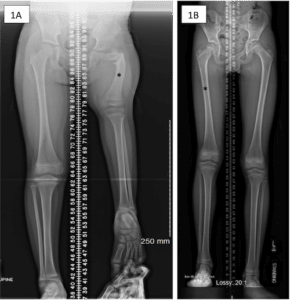
Proximal femoral focal deficiency and congenital short femur are thought to be versions of the same problem, also known as congenital femoral deficiency. These conditions both affect the femur (the thigh bone). With congenital short femur, the bone can appear almost normal on an x-ray. However, it is shorter than the other side. In some children, the difference in length is not noticed until they are a few years old or even until adolescence. However, in other children, the leg length difference can be noticed shortly after birth (Figure 1).
Figure 1: (A) This is an x-ray of the both legs of a 4 year old female with proximal femoral focal deficiency. Notice that the left leg is much shorter than the right and that the shape of the left femur (noted by *) is very different than the right. (B) 11 year old male with right congenital short femur. Unlike 1A, the right femur in this child (*) looks very similar to the left side and he has only a 4.5cm difference in the length of his right leg compared to the left.
With proximal femoral focal deficiency, the femur shape is also affected and can be significantly shorter than the other side. On x-ray, the portion of the femur that is closer to the hip joint can appear severely angled, it may be mostly made of cartilage and therefore difficult to see on an x-ray when a child is very young, or the proximal femur may be absent (Figure 2). Congenital short femur and proximal femoral focal deficiency are thought to be part of the same spectrum of pathology, with congenital short femur often being less severe than proximal femoral focal deficiency. The following article is meant to be a brief overview of these diagnoses and potential treatment options and is not meant to be a comprehensive review of all possible surgical and nonsurgical treatments.
Figure 2: Pelvis x-ray of a 2 year old female with severe left proximal femoral focal deficiency, where the proximal portion of the left femur did not develop.

Cause
The cause of proximal femoral focal deficiency and congenital short femur is not known. It is thought that these disorders may be due to one or more genetic mutations that affect limb development but this has not been proven.
Symptoms
The child generally does not have pain in the hip, leg or knee. Usually the first thing that a child or parent notices is that the affected leg is shorter than the other leg. If this difference is mild, the child may not present until much later in childhood or adolescence. If there is a more significant difference in the length of the femur bone, this will be noticed at a younger age.
Doctor Examination
Congenital short femur and proximal femoral focal deficiency are associated with lateral longitudinal deficiencies of the leg. This means that the most lateral (outer) portion of the bones in the leg can be affected in these patients. Therefore, it very common for children with either congenital short femur or proximal femoral focal deficiencies to have other conditions aside from just a leg length difference. These changes affect the alignment of the leg overall including the development of knee ligaments. It is not uncommon for the lower leg (below the knee) to be affected as well, in which case the lower leg generally has fibular hemimelia.
Children with proximal femoral focal deficiency can have delayed development of the proximal portion of the femur, which affects hip development. When the bone does develop, it is often significantly angled and rotated. The hip socket may not be appropriately deep (this is called acetabular dysplasia). In children with severe proximal femoral focal deficiency, the proximal femur may never form. The severity of the disease often dictates how the leg moves at the level of the hip joint and it generally related to the severity of the leg length difference. On exam, these children often have a shorter, bulkier thigh.
Children with congenital short femur can have a leg which looks very similar to the other side, but shorter. The hip often moves in a way that is similar to the other side with regards to flexion, extension and rotation, but the thigh itself is shorter in length and may have a smaller width as well.
Children with PFFD and CSF are also more likely to be knock-kneed on the side of the PFFD/CSF. This is called genu valgum. This deformity develops because the outside portion (lateral condyle) of the end of the femur tends to be smaller and less well developed than the inside portion (medial condyle). This can get worse with growth. Having a child stand with blocks under his or her foot on the side of the PFFD/CSF is a way to clinically determine the length difference between the normal leg and the leg with PFFD/CSF. This also allows the physician to better visualize and appreciate the severity of the knock-knee (valgus) deformity on the side of the PFFD/CSF compared to the normal side. Your physician will likely also get a standing lower extremity x-ray of both legs, with the same size blocks under the PFFD/CSF sided foot as a way to measure on x-rays both the length difference and angular difference between the legs (Figure 3).
Figure 3 Leg length x-rays of a 4 year old girl with congenital femoral deficiency standing on blocks to evaluate her leg length difference and knee valgus. Image courtesy of Jaclyn Hill, MD

Both children with proximal femoral focal deficiency and congenital short femur can be born missing one or more ligaments that help stabilize the knee joint. Often, these children will be born without an anterior cruciate ligament (ACL). You physician will do a thorough examination of both knee joints to determine if the knee on the side the of PFFD or CSF is different from the knee on the unaffected leg.
Your physician will also assess the lower leg and foot for signs of fibular hemimelia, as this is commonly associated with PFFD/CSF.
In addition, PFFD/CSF can be seen in combination with other medical syndromes. Therefore, you physician will do a complete examination of your child. This will include evaluating your child’s arms and hands to look for other congenital problems, in addition to the other leg. Children with PFFD/CSF on both sides sometimes have associated facial changes. Your physician will check your child’s back for scoliosis and may get x-rays to evaluate for this as well.
Treatment
Treatment depends on the condition that your child has as well as the severity of the condition. Children who have only a mild form congenital short femur, with a normal knee, leg, ankle and foot, are treated very differently from children who have severe proximal femoral focal deficiency, absence of knee ligaments, fibular hemimelia, and an abnormal and stiff foot and ankle.
The main treatment approaches include either limb lengthening and reconstruction or use of a lift and/or prosthetic, with or without amputation of a portion of the limb.
Surgical reconstruction is complex and varies a great amount from child to child. The overall treatment plan will be based off discussions that you have with your child’s surgeon. It is easier to understand the treatment plan when one considers the separate goals of surgery. Overall, the goals of treating congenital femoral deficiency are maximizing hip function, maximizing knee function, and equalizing limb lengths. Treatment of the lower leg and foot are discussed in the section on fibular hemimelia.
Maximizing Hip Function
Children with PFFD often require a reconstruction of the proximal femur to release muscles and tissues that are abnormally tight, correct the angular and rotational deformity of the proximal portion of the femur and surgery on the pelvis to make sure that the hip socket appropriately covers the femoral head. This is referred to as a SUPER hip procedure and can be the first step of limb reconstruction and lengthening in children with PFFD because appropriate formation and alignment of the hip joint is essential if limb lengthening is going to be pursued.
Maximizing Knee Function
Children with large predicted leg length differences who are missing one or more of the stabilizing ligaments in the knee may benefit from ligament reconstruction prior to limb lengthening. This improves the stability of the knee and can help prevent the knee from dislocating during the lengthening process, which is a real and serious risk of limb lengthening in this population.
Children who have a knock-knee (valgus) deformity, may require correction of this either with a procedure known as guided growth or with an acute femoral osteotomy. Guided growth uses small plates to tether the growth plate of the femur, allowing the bone to “grow” itself straight over time (Figure 4A). A femoral osteotomy means that the bone is cut and corrected to the new position, then held in this new position while it heals either with a plate/screw construct or with an external fixator (Figure 4B).
Figure 4: (A) This is an 11 year old female with mild knock-knee knee deformity which was treated with growth modulation. This is useful in children with mild deformities who still have open growth plates. As the bone grows, the plate acts like a rubber band and allows the bone to gradually grow straight. (B) A mature adolescent with the same deformity. She was not a candidate for growth modulation because her growth plates were closed so she underwent an osteotomy with a plate and screws.
4A

4B

Equalizing Limb Lengths
Based on the examination and x-rays tests discussed above your physician will try to predict how large the leg length difference would be when your child is an adult, if no surgery was done. The larger the predicted difference between your child’s leg lengths, the more likely that your child will need more than one lengthening procedure to achieve equal leg lengths at maturity. Shortening procedures of the normal extremity (epiphyseodesis) may be recommended to equalize the LLD.
The lengthening of the bones can occur either with an external fixator or with an internal lengthening nail. Both devices require a surgery to position either the intramedullary nail or the external fixator and cut the bone. The advantage of the nail is the implant is completely inside the body while the pins and/or wires of the external fixator stick out of the skin. The advantage of the external fixator is that it can be used in younger children who need multiple lengthenings, and because it has more ability to make large corrections in bone shape. Patients who have had lengthenings with both devices often prefer to have the intramedullary nail due to the inconvenience of the external fixator. Patients with external fixators are more likely to have skin complications due to infections at the pin and wire sites. However, as the bone is lengthened, both devices are also lengthening the surrounding muscle, blood vessels, nerves and skin. Therefore, both devices have the same rates of other complications seen in lengthening procedures, including muscle contractures and joint dislocations.
The lengthening process happens slowly and usually requires weekly or biweekly visits with your surgeon to monitor how the bone is lengthening as well as to check and make sure that your child is not developing a muscle contracture or having problems at either the hip or knee joint due to the lengthening. It also requires regular physical therapy and home stretching and rehabilitation exercises daily, and often brace wear daily, to prevent problems during the lengthening such as muscle contractures or joint dislocation.
An alternative to limb lengthening and reconstruction is use of a prosthesis, with or without limb lengthening. This may be something small, like a short lift used inside or attached to the outside of the shoe. This can work well for patients who have very small differences between their leg lengths. Children with larger leg length differences whose families do not want surgery or are not ready for surgery can walk in with a specialized prosthesis. Children with severe PFFD or PFFD associated with severe ankle and/or foot abnormalities that are not amenable to reconstruction or do not want to consider multiple surgeries may be treated with an amputation of the foot through the ankle joint, although the hip and knee may still need treatment. Children with severe PFFD but who have a normal ankle and foot may be candidates for a procedure called rotationplasty, where the child’s ankle is reconfigured to function as a knee.
The decision to pursue limb lengthening and reconstruction versus amputation and use of a prosthetic is a deeply personal decision. It depends on your child’s diagnosis, the predicted difficulty of limb lengthening and reconstruction, and your and your child’s preferences regarding surgeries and overall goals for treatment. If possible, it is often helpful to have your child see multiple surgeons so that you and your child can hear multiple opinions about the risks and benefits of potential treatment plans. The surgeon who cares for your child with PFFD/CSF is often the surgeon who follows your child for as long as he or she is growing and may be doing multiple surgeries on your child regardless of the treatment approach that you choose. It is critical that you choose a physician with whom you and your child are comfortable and who you trust.
Outcomes
Outcomes of treatment depend on the type of surgery (or surgeries) that your child has. Standard complications with orthopaedic surgeries include problems with the skin or bone healing. If your child is undergoing a lengthening procedure of one or more bones, the skin, muscle, and all of the soft tissue structures around the bone are also being lengthened. The lengthening process puts stress on the joints above and below the bone that is being lengthened as well (for example, if your child is having his or her femur lengthened, this process will put stress on your child’s hip and knee joint). Lengthening can cause the surrounding muscles to tighten so much that muscle contractures (fixed tightness of the muscles) can develop and joints, specifically the knee and hip joint, can dislocate during the lengthening process. Therefore, the lengthening is done slowly and usually in combination with aggressive bracing and rehabilitation to prevent these complications. Additional details for each procedure are available on this website. Complications relating to amputation depends on what type of amputation that your child would have. Skin related complications and problems with prosthetic fit can occur.
Take Home
There is no one single treatment approach for children with PFFD or CSF. Often, the diagnosis can be made at a very young age, when the child is only a few weeks or months old. Many of the treatment options that have been reviewed are not initiated until the child is at least 1 year of age or older. It is important not to rush into a treatment with a specific provider. Your child has been born with a leg that is different than other children but this does not mean that your child will not crawl, walk, run or jump. Taking time to find out more information, explore treatment options and even talk to multiple providers about what a treatment plan would look like for your child is not going to delay your child’s development. Making sure that you are comfortable with your surgeon and that you are making the treatment decision that works best for your child and your family is a critical first step, regardless of what treatment path you pursue.