External Fixation in Pilon Fractures
Ahmed Thabet, M.D.
Texas Tech Health Science Center at El Paso
Introduction:
The lower end of the shin bone (tibia) is a part of the ankle joint. This part of the tibia looks a like a ceiling and frequently called the tibia “plafond” or “pilon”. The ankle joint has crucial role in normal walking function. Any disturbances of the ankle joint range of motion or joint surface shape may cause limping with severe functional limitations.
Description:
Pilon fractures damage the distal tibia joint region (articular region). The joint surface can be partially or totally affected. The more damage to the joint surface, the more difficult it is to assemble the joint pieces and the more risk for rapid degeneration of the ankle joint. This is called early posttraumatic arthritis, a condition that is a well known consequence of these types of injuries when severe enough. The impact of the trauma does not only involve the bone but extends to soft tissues around the ankle. Severe swelling, blood filled blisters and open wounds are very common and add to the complexity of the injury. Wound infection, wound breakdown, non healing of fractures, or healing in a crooked position can compromise the outcome. In severe cases these fractures can end up with the need for fusion (forcing the tibia and bone below it to become one combined bone) or even for below knee amputation.
Causes:
1- Fall from height, such as a ladder or roof
2- Motor vehicle collision (MVC)
Symptoms:
This fracture can happen in isolation or combined with other injuries. A complete patient evaluation is critical to avoid missing any other fractures. The patient usually reports severe pain, swelling and a visibly crooked ankle after falling from a roof or ladder.
Doctor Examination:
The focused exam on the ankle usually reveals severe swelling, blood-filed blisters and the ankle in a crooked position. Evaluation for any compromise to blood flow (pulses), sensation of the foot and any open skin wounds is very important.
Treatment:
The treatment options vary according to soft tissues factors, fracture factors, patient factors, and surgeon preference. The treatment can be two stages (two separate surgeries) or one stage. Each option has its advantages and limitation
• The two-stage option is the most common approach. The severe swelling, blisters and open wounds increase the risk of surgical site infection and wound breakdown if the fracture is surgically fixed right away. The degree of involvement of the joint surfaces may need extensive surgical exposure of the joint from the front and back. The two stage approach includes application a temporary ankle spanning external fixator for one or two weeks followed by removal of the external fixator, manipulation of the fracture into an ideal placement, and placement of plates and screws to hold its position. Bone graft may be required to fill in areas where bone was crushed and impacted. The time in the spanning external fixator allows the swelling to come down and for soft tissue healing. This decreases the risk of wound healing complications and minimizes the risk of surgical site infection.
• An alternative option is one stage approach. A circular external fixator with rings around the ankle can be used from outside to fix the fracture. Restoration of the joint surface is performed with small incisions with the use of screws or wires to hold the bone. The ring external fixator is then applied. The external fixator fixation may or may not extend the foot. This depends on the length of the lower end of the tibia available for fixation. This option is limited by pin site infection (generally treatable with local wound care and antibiotics) and the inconvenience of the external fixator. It has the benefits of early walking and the ability to treat fractures with severe soft tissue damage.
Outcomes:
The outcomes of these types of fracture can be good, although complications rates can be higher in more complex injuries. Residual stiffness and difficulty using the ankle may be experienced and require continued care by your surgeon.
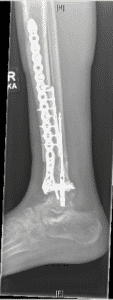
Figure 1
A 51 year old male suffered a fall from 10 feet and suffered a closed pilon fracture (1A/B). His injuries were treated in a staged fashion with an external fixator (1C) and then after his swelling improved, the external fixator was removed and plate and screws were used to reconstruct the broken pieces and bone graft placed in an area of crushed bone (1D/E)
1A

1B

1C

1D

1E